
OPENING UP: The D-Termined Program has been used as an effective tool to enhance efforts by the dental team to guide the behavior of children with ASD. Using both the remote and physical dental office setting, the same principles of behavior guidance apply to overcome barriers that the COVID-19 circumstances have presented.
YES! DENTAL APPOINTMENTS CAN BE SUCCESSFUL:
MODIFYING THE D-TERMINED PROGRAM™ OF FAMILIARIZATION & REPETITIVE TASKING TO THE COVID-19 PANDEMIC CIRCUMSTANCES
BY DAVID A. TESINI DMD, MS AND AMY LUEDEMANN-LAZAR, DDS, MS
INTRODUCTION
Yes! Children with special health care needs (CSHCN) have difficulty accessing quality, comprehensive dental care. The barriers of finding trained and willing providers, negotiating hurdles of Medicaid and insurance company coverage, and just plain balancing jobs, family and other activities of daily living, often make this an unsurmountable challenge. COVID-19 has magnified these difficulties and heightened the barriers. The result: many children with special healthcare needs (CSHCN) are being recommended for general anesthesia in the hospital or out-patient setting because it is mistakenly viewed as the easiest and best route during the COVID-19 pandemic. But, with our understanding of how children with autism spectrum disorder (ASD) learn in school and educational settings, dentists can adapt these learning concepts to the dental office and avoid retreating to the use of general anesthesia. COVID-19 has given us this opportunity to innovate and adapt behavior guidance techniques to the digital transformation without the use of sedation or general anesthesia.
One such technique is the D-Termined Program,™ a behavior guidance approach that uses Applied Behavior Analysis (ABA) to prepare children for a dental visit. This encourages desensitization through familiarization without the use of protective stabilization, sedation, or general anesthesia. Modified for the COVID19 pandemic circumstances, this program is practiced at home and applied in the dental office. With practice, families and dentists can use teledentistry and video communication, in combination with the D-Termined Program, to help children with ASD and other disabilities succeed in the dental office setting.
Virtual conferencing, video communication, and teledentistry are enhancing the traditional models of care delivery. For children with ASD and related disorders, the challenges for successful transition to these methods may be initially difficult, but in the end surprisingly successful. With knowledge of how children with ASD learn, and by understanding their social behavior, dentists can innovate to make routine dental care available to all children with challenging behaviors. We cannot let the disability eclipse the need for dental care.
ABA AND DENTAL DESENSITIZATION: A WINNING TEAM
Our fear is that preventive and routine dental care for CSHCN will be postponed until dental office protocols become more familiar for both patients and staff. Children are seen "waiting for an opening" for their "turn" for a general anesthesia appointment. There is a growing concern, if behavior guidance approaches, and utilizing teledentistry and innovation are not quickly integrated into dental offices, special care dentistry could be set back by decades.
Applied Behavior Analysis (ABA) therapy utilizes learning theories to modify behavior, most specifically social behaviors. This therapy has been shown effective for children with ASD, by creating new behaviors, refining already acquired behaviors or skills, and decreasing disruptive behaviors. This therapy uses communication, repetition, and reward as cornerstones in behavior shaping. The D-Termined Program of familiarization and repetitive tasking is based on these principles.
A study at Tufts Dental School in Boston (AlHumaid et al 2016) showed that the D-Termined Program can reduce the need for general anesthesia. This involved frequent office visits of desensitization which is not practical in the present COVID-19 circumstances. Fortunately, learning mechanisms of ABA that are central to the D-Termined Program are adaptable to remote learning and teledentistry. This gives us an opportunity to innovate our past behavior guidance approaches by integrating video communication and video conferencing (VC).
IMPROVING OUR UNDERSTANDING OF THE "AUTISM PERSPECTIVE"
When we lecture, we always point out that "it is more about understanding behavior than managing behavior." As parents and dentists, we work hard to understand the "autism perspective". It is a call for us to "get into their world." Impairment in social interaction, communication skills and sensory processing disorders can combine with anxiety and dyspraxia to create difficulty for dentists to design behavior guidance approaches. The COVID-19 crisis has magnified this challenge. Some behaviors become rooted and repetitive, so emphasis needs to be directed to recognize these behaviors before they form. Communication between the patient, parent, caregiver, therapist, and dental provider will help us to manage these concerns.
Parents have successfully used ABA procedures through homebased learning formats and telehealth (Lindgren et al., 2016). Telehealth as a service delivery mechanism depends on parent participation and dentist training with dependable follow through. These models of training are then integrated into the DTermined Program. The first visits, typically the most important in any training process, are followed by component tasks that are then delegated with instruction for parent and child to do "between visit homework."
WHAT IS THE D-TERMINED PROGRAM OF FAMILIARIZATION AND REPETITIVE TASKING?
The D-Termined Program of Familiarization and Repetitive Tasking uses desensitization through repetitive tasking in a structured learning sequence (Tesini DA, 2014). As in ABA theory, this method systematically applies the principles of behavior analysis in order to identify the variables that improve social behavior It uses visual icons and verbal cues (see figure 1).
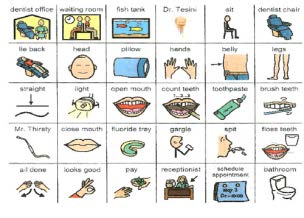
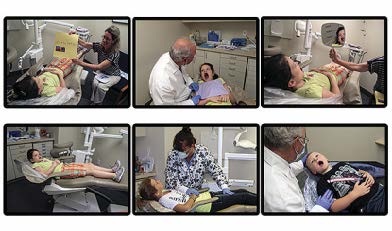

FIGURE 1: Icons for story book, positional modeling photo card and iconic counting framework
Repetition and familiarization form the basis of this non-pharmacological behavior guidance approach. Three repetition factors are the keys to success.
1."Look at me" for eye contact
2."Put your feet out straight and hands on your tummy" for positional modeling (Figure 1)
3.Use of a counting framework "1.2.3.4.5.6…." verbal or visual (counting charts)
As the patient learns the use of these repetitive commands, the dental provider can now simply follow the five major principles of the D -Termined Program:
1) Divide the Skill (Tasking chart figure 4)
2) Demonstrate the Skill
3) Drill the Skill
4) Delegate the Repetition
5) Delight the Learner.
We are fortunate that both training videos and supplemental support materials are available on the internet. Videos provide a great resource for orientation of the parents and training of dental staff: ( specializedcare.com/collections/educational-products/products/d-termined- program-for-patients-with-autism)
BUT HOW DO WE MODIFY THE D-TERMINED PROGRAM FOR COVID-19 PANDEMIC CIRCUMSTANCES?
Modifications of the D-Termined Program, utilizing teledentistry combined with traditional office visits may at first be met with trepidation by the dental team. Drs. Lindgren and Wacker from the University of Iowa reported in 2016 that ABA telehealth can in fact, be used effectively to successfully communicate and teach skills of behavior guidance. It succeeds because parents of children with ASD already understand these challenges and are already making necessary adjustments with school, recreation, and other gap activities for their child.
The five basic principles of the D-Termined Program are modified and integrated between a virtual and physical world. A precedent videoconference consult with parents is important to define the objectives and timeline and introduction with patient. Include a picture of you with the patient, if seen previously in the office. Be aware that the training for parents and patient is time sensitive in periodicity and must be planned within the context of other ADL (Activities of Daily Living). The initial teledentistry appointment can be used to introduce exaggerated PPE and infection controll guidelines so it will not interfere with developing behavior guidance protocols The number of visits dedicated to learning the repetitions of "feet out straight, hands on tummy and counting framework" through videoconferencing will vary from patient to patient (see figure 2).

FIGURE 2: Teledentistry and video communication training tailored to patient centered D-Termined Program training.
After the telehealth training visits, based on patient progress, the decision on when to schedule the first physical office setting appointment can then be made. This will vary from patient to patient and is always subject to modification. An initial approach for continuity in the training would be to schedule four telehealth, two in-office and a final telehealth appointment, with defined objectives for each visit.
Teledentistry 1: Parents Consult VC: Narrated 'Preview Video', Communication (The picture book, "Look at me", "Positional modeling" and a "Counting Framework"
Teledentistry 2: Patient Centered VC: Introduce PPE, Picture Book, Communication. "Look at me", "Positional modeling" and a "Counting Framework".
Teledentistry 3: : Patient Centered VC: Tasking Chart in Progressive tasks
Teledentistry 4: Patient Centered VC: Repetition as necessary
Physical Office 5: Patient in-office Visit #1: Tasking Chart
Physical Office 6: Patient in-office Visit #2: Tasking Chart to Prophy and Fluoride
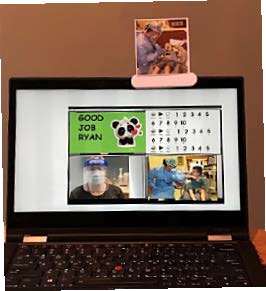
FIGURES 3 & 4: There are opportunities to enhance the videoaudio communication experience with advancing knowledge of the use of video conferencing applications (apps) and computer attachments for visual support directly to the computer screen; Adjunctive Visual icons. Power Point "share screen" with photo clip attached to top of the patient's computer screen.
Again, the repetition of directions and requests that form the cornerstone of the D-Termined training, (i.e., "feet out straight", "hands on your tummy" and using the counting framework) are readily adapted and critical to virtual training with audio and screen-time technology. There are opportunities to enhance the video-audio communication experience with advancing knowledge of the use of video conferencing applications (apps) and computer attachments for visual support directly to the computer screen (see figure 3). Teledentistry visits can include lessons prepared in power point and using "shared screen" on the VC application. Innovation can include the use of videos, in-meeting chat and recording content.
Between visits and training with the parent, classroom teacher, and/or behavioral therapist become critical to the patient by learning through continuity and repetitive tasking; "eye contact … feet out straight… counting framework". Ordering and structuring of video conferencing and in-office visits can be reviewed and modified with all participants and agreed upon as the program progresses. The tasking sheet will serve as a guide to planning these visits (see figure 5).
Training of the dental office staff is important for the long-term success of the D-Termined Program. The dentist must "delegate the repetition" in order for this program to be successfully integrated into the dental office. Parents can involve dentists, teachers, and therapists to assure that their child has access to this program. Accolades for all on social media must not be underestimated as a wonderful motivator.
THE BOTTOM LINE IS TO GET THE WORD OUT
The D-Termined Program has been used as an effective tool to enhance efforts by the dental team to guide the
behavior of children with ASD. Using both the remote and physical dental office setting, the same principles of behavior guidance apply to overcome barriers that the COVID-19 circumstances have presented. Innovation and planning at first may seem overwhelming, but with a structured approach and between-visit parental and care- giver training, the methods used in ABA learning can be adapted to providing dental care to children with special healthcare needs.
Each office can customize the benefits of telehealth to their patient needs. Both parents and the dental team must be determined to succeed.•

FIGURE 5: Generic Tasking Chart; Hash lines are used to set landmarks for each in-office visit.
Acknowledgements: The Nancy Laurie Marks Foundation Brookline MA. funded the original instructional videos, which have been used for training parents, dentists, and staff since 2004. Suzy Yankowitz, RDH and parent, for her help and advice with video communication. The videos are distributed by Specialized Care Corporation Hampton, NH. ((800) 722-7375) and are available to preview through their website vimeo.com/443140616
ABOUT THE AUTHOR:
David A Tesini DMD, MS is Associate Clinical Professor TUSDM; affiliated with Tesini Pediatric Dentistry based in Hopkinton, MA. Dr. Amy Luedemann-Lazar is a board-certified pediatric dentist. She earned a DDS degree from the University of Texas and a master's degree from the University of Washington in Seattle. She worked at Seattle Children's Hospital and taught at the University of Washington, serving on the craniofacial team and working extensively with children who had special health care needs. She believes in giving back and helping those in need and has been on numerous medical/dental mission trips around the world.