EVALUATION AND MANAGEMENT OF OBESITY IN ADULTS WITH INTELLECTUAL DISABILITY
BY PHILIP MAY M.D.

Obesity, which is usually defined as Body Mass Index (BMI) of equal to or greater than 30 kg/m2, has become a serious health risk for many individuals and groups in the United States and worldwide. The US Surgeon General has declared that obesity has reached epidemic proportions and has called for immediate action designed to prevent and reduce the impact of this condition on the individual and society at large.
Obesity in the general population has been shown to be associated with highrisk for hypertension, diabetes, dyslipidemia, heart disease (both atherosclerotic cardiovascular disease and diastolic heart failure), osteoarthritis, sleep apnea, pneumonia, gallbladder disease, liver disease, 13 different cancers (e.g., endometrial, breast, colon, and others), and gynecological problems (abnormal menstrual periods, infertility). Obesity has also been shown to have adverse effects on brain anatomy and function, resulting in abnormalities of cognition, mood, and behavior.
Limited research has demonstrated that obesity is a major health threat for persons with Intellectual and Developmental Disabilities (IDD) as well as for the general population (see Table 1, next page). Prevalence of obesity is 40-50% in various surveys for both men and women with IDD who live in the community. The cause of obesity in persons with IDD appears to be multifactorial and related to various genetic and environmental factors (see Table 2). It has been shown that "mild" IDD, community residential status, and young age are all related to an increased risk for obesity in persons with IDD. Certain medications, especially second-generation antipsychotics, also appear to convey an increased risk for obesity. Obesity in persons with IDD can limit opportunities for community participation such as employment and leisure, require more effort on the part of caregivers in assisting individuals with IDD with various activities of daily living, and result in higher medical costs related to treatment of obesity-related health conditions, all of which can lead to a greater mortality rate and reduced life-expectancy for this medically underserved and vulnerable population of U.S. citizens. Currently, obesity has also been shown to be associated with increased morbidity and mortality from COVID-19 infection1, and this effect may be even greater for individuals with ID.2
Table 1. Complications of Obesity in Adults with Intellectual Disability
• Associated with higher mortality rates and shorter life expectancy
• Increased rate of diabetes, dyslipidemia, hypertension, sleep apnea, arthritis.
• Increased Cardiovascular Disease (Heart attacks, Strokes, PVD)
• Increased Gallbladder Disease and Gallstones
• Increased incidence of Gout
• Increased Periodontal Disease
• Increased risk for Cancer
• Abnormalities of brain structure (atrophy) and function (worse Cognition, Mood and Behavior)
• Increased risk of morbidity and mortality from COVID-19 Infection
Treatment of Obesity
In the general population, treatment of obesity is usually accomplished by behavioral/lifestyle approaches, medications, and/or surgery. Barriers to treatment of obesity encountered in adults with Intellectual Disabilities include sparse curriculum in Medical Schools and lack of research which addresses how best to evaluate and manage those health conditions (such as obesity) that frequently occur in adult men and women with IDD. Few physicians have experience regarding evaluation and management of health conditions, such as obesity, in adults with ID. This often results in "fragmentation" of care delivered by multiple specialists who do not communicate. For example, a psychiatrist may be prescribing an obesogenic psychotropic medication (e.g., olanzapine) for behavior with undocumented benefit, while an endocrinologist, without collaboration with the psychiatrist, might prescribe topiramate for obesity, which may also have a psychotropic benefit better than olanzapine. Both psychiatrist and endocrinologist need to communicate with each other, and with the primary care provider, who needs to ensure that this communication occurs.
Table 2. Causes of Obesity in Adults with ID
1. Socio-environmental: Food used as reinforcer for good behavior, boredom.
2. Genetic: e.g., Prader Willi Syndrome
3. Metabolic: e.g., Cushing's Syndrome, Hypothyroidism
4. Medication Side Effects: e.g., Neuroleptic medication
5. Psychiatric: "Food Addiction"
6. Sedentary behavior
Effective treatments of obesity in the general population exist. These include non-pharmacologic/non-surgical ("lifestyle"), pharmacologic, and surgical approaches. Non-pharmacologic/non-surgical approaches include various combinations of nutrition, exercise, and behavior modification programs. Reports of purely pharmacological and surgical treatments of obesity are not as common as the "lifestyle" approaches in treating obesity in adults with IDD. A recent US Preventive Services Task Force-commissioned literature review concludes that behavioral counseling interventions to promote combined lower calorie diet (500 Kcal/day reduction) and more exercise (150 minutes/week) produce a statistically significant reduction in cardiovascular risk factors (including obesity) at 12-24 months 3. However, the relative contributions of diet vs. exercise, the importance of weight-loss, and the specific role of the primary care physician in this "behavioral" approach to reduction of cardiovascular risk factors (including obesity) have still not been clarified. It seems likely in most cases of behavioral treatment of overweight status, if significant weight-loss occurs, and is maintained, multiple cardiovascular risk factors (such as diabetes, high cholesterol, hypertension) will improve or even disap pear completely without use of medications or surgery.
Table 3. Components of an Effective Quality Improvement "Fitness Program" for adults with IDD
1."Meaningful" individualized Daily Physical Exercise Program (Establish the "Habit").
2. Dietary: Reduced caloric intake & increased protein.
3. Supportive and Trained Staff and Caregivers.
4. Frequent Medical and Administrative Follow-up.
5. Documentation of Benefit to provide feedback to persons with IDD and their caregivers.
• Body Composition Analysis of muscle and adipose tissue.
• Routine metabolic tests (e.g., fasting blood glucose, A1C, lipids)
• Baseline and Follow-up Psychometric Testing for cognition, mood, and behavior
• Individualized Exercise Program prescribed and monitored by physician and monitored with an activity measuring device (Steps-per-Day).
• Statistical Analysis to determine efficacy of interventions for feedback information for administration, staff, and participants of the QI Program.
It has been noted by others that primary care physicians (for multiple reasons), while adequately medically addressing weight-related "complications" such as diabetes, dyslipidemia, hypertension, sleep apnea, etc., rarely provide CMS-recommended "behavioral" (non-drug or surgical) treatment of "obesity itself".3 In a recent JAMA interview,4 Popkin commented that the specific issue of "obesity itself" has been relatively ignored by physicians and policymakers, when compared to attention given to the many "complications" of obesity (such as diabetes, hypertension, coronary heart disease, and even increased morbidity and mortality from COVID-19 infection). These same issues are also observed in treating obesity in patients with IDD.
While a lower calorie diet alone has been shown to be effective for weight-loss short term (< 3 years), the preponderance of evidence suggests that very few people with obesity can maintain weight-loss by caloric restriction alone for more that 2-3 years. Long-term success (> 9 years) is more likely to occur in those obese individuals who exercise regularly.6 This might be explained by the fact that people with obesity characteristically have reduction of volume of certain areas of the brain ("hippocampal hypovolemia") which can cause both cognitive and mood disorders. Physical exercise has been shown to stimulate neurogenesis of hippocampal neurons by exercise-induced increased production of both brain and skeletal-muscle Brain Derived Neurotrophic Factor (BDNF), which then leads to improved mood and less emotion-driven compulsive eating.7
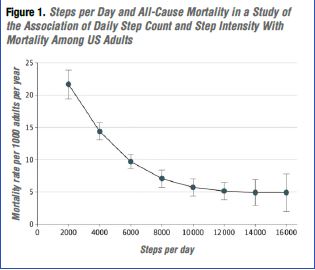
Thus, maintenance of weight loss and subsequent CVD risk factor reduction long-term may primarily be a problem of "the head not the scale" that needs to be addressed with the "habit" of daily exercise see Figure 1, before long-term weight loss and metabolic/CVD risk-reduction can occur.8 Physicians could play a key role in this process if they required that "behavioral" treatments were in place before the "pills" were prescribed.
Health agencies and governments could also be supportive by encouraging health provider organizations/clinics to establish Quality Improvement Programs9 focused on obesity treatment. (see Table 3). Quality Improvement "fitness programs" have been shown to reduce incidence of metabolic problems (diabetes, dyslipidemia), increase muscle mass and function (treatment of sarcopenia), correct hypertension and sleep apnea, reduce risk for cardiovascular disease and cancer, improve cognition, mood, and behavior and reduce polypharmacy.•
ABOUT THE AUTHOR:
Philip May M.D. is Director of Quality Improvement Program Development, International Foundation for Chronic Disabilities, Louisville, KY.
References
1. Abbas, A., Fahey, s., Fawzy, A., Salem, A., & Shawky, M. (2020) The Mutual Effects of COVID-19 and Obesity, Obesity Medicine, 19, doi.org/10.1016/j.obmed.2020.100250
2. Turk, M., Landes, S., Formica, M., & Goss, K. (2020) Intellectual and Developmental Disability and COVID-19 Case-Fatality Trends: TriNetX Analysis, Disability and Health Journal, 13, doi.org/10.1016/j.dhjo.2020.100942
3. O'Conner E, Evans C, Rushkin M, et al. Behavioral Counseling to Promote a Healthy Diet and Physical Activity for Cardiovascular Disease Prevention in Adults with Cardiovascular Risk Factors: Updated Evidence Report and Systematic Review for the US Preventive Services Task Force. JAMA. 2020; 324: 2076-2094.
4. Omura J, Bellissimo M, Watson K, et al. Primary care providers' physical activity counseling and referral practices and barriers for cardiovascular disease prevention. Preventive Medicine. 2018; 108: 115-122.
5. Abbasi, J. Large Meta-Analysis Digs into Obesity's COVID-Risks, JAMA. 2020; 324:1709.
6. Church, T, & Martin, C. Exercise is the Key to Keeping Weight Off, But What is the Key to Consistently Exercising?, Obesity. 2019; 27: 361.
7. Rendeiro, C., & Rhodes, J. A New Perspective of the Hippocampus in the Origin of Exercise-Brain Steps per day Interactions, Brain Structure and Function. 2018; 223: 2527-2545.
8. Saint-Maurice, P., Troiano, R., Bassett, D., et. al. (2020) Association of Daily Step Count and Step Intensity with Mortality Among US Adults, Journal of the American Medical Association, 323, 1151-1160.
9. US Dept of Health & Human Services Training Module, Quality Improvement, April 2011. hrsa.gov/sites/default/files/quality/toolbox/508pdfs/developingqiplan.pdf