COVID-19 & ADULTS WITH INTELLECTUAL DISABILITY, AUTISM, EPILEPSY, OR BRAIN INJURIES
FINDINGS FROM AN ONLINE SURVEY
BY CHARLES E. DRUM, MPA, JD, PHD., ANTHONY OBERG, MA, JACOB DITSCH, OTD, KARL COOPER, JD AND ROBERTA CARLIN, MS, MA, JD
INTRODUCTION
People with disabilities, including persons with intellectual and developmental disabilities (IDD), experience unique risks during emergencies, disasters, epidemics, and pandemics that can impact health and health care (White, 2009). Yet, little is known about the full impact of COVID-19 on people with disabilities. The American Association on Health and Disability (AAHD) conducted the COVID-19 & Disability Online Survey to obtain rapid, realtime information on the coronavirus pandemic's impact on adults with a range of disabilities. We used four of the American Community Survey's disability identifiers (Vision, Hearing, Mobility, Difficulty Concentrating, Remembering or Making Decisions). Respondents could also identify if an intellectual disability, autism, epilepsy, or brain injury was the underlying condition that caused the difficulty concentrating, remembering, or making decisions (other response options were available, too).
ABOUT AAHD
The mission of the American Association on Health and Disability (AAHD) is to promote the health and wellness of children and adults with disabilities and reduce health disparities. AAHD achieves this by advocating for community inclusion and promoting full accessibility, integrating disability into the public health agenda, advancing disability research and knowledge translation, and conducting training and advocacy.
METHODOLOGY
Existing COVID-19 surveys were reviewed and items were either modified or new ones created. Items included demographic questions (disability identifiers, gender, ethnicity, race, geographic area, and type of health insurance), questions on COVID-19 information and impact and access to regular (non-COVID-19) health care and services. Survey responses were solicited through AAHD's dissemination networks and through existing partnerships. The survey was available online from April 17, 2020, until May 1, 2020.
RESULTS
This article summarizes results from a report that focused on respondents with an intellectual disability, autism, epilepsy, or brain injuries.'Additional reports by different disability types and a summary report are also available. Survey completion rates varied by item, ranging from a low of 88% to 100%, with an overall completion rate of 94% (exclusive of skip patterns). Descriptive statistical results are summarized below.'
DEMOGRAPHICS
Out of a total of 2,469 respondents, 930 reported experiencing serious difficulties concentrating, remembering, or making decisions due to an intellectual disability, autism, epilepsy, or brain injury (38%). The majority of the respondents were 18-44 (80%), followed by adults that were 45-64 (18%), and adults 65 and older (2%). The majority of adult respondents were either Female (59%) or Male (37%). The sample was primarily White (79%), followed by Black or African-American (11%), Hispanic (5%), Asian (4%), American Indian or Alaska Native (2%), and Native Hawaiian or Other Pacific Islander (0%). Respondents selected their location as Urban (19%), Suburban (57%), Rural (23%), or Frontier (0%). Respondents reported having Medicaid/CHIP (68%), Medicare (40%), Private Insurance (31%), VA/Government insurance (6%), and Other (5%), although respondents could select "all that apply." One percent of respondents had no insurance.
COVID-19 INFORMATION SOURCES
Respondents were asked to rank their three most important sources of information about COVID-19 out of nine options. As displayed in Table 1, among the nine information sources, the three most important were Relatives (31%), Television (29%), and the Internet (15%). Respondents identified the Television (27%), the Internet (20%), and Relatives (14%) as the three second most important sources of information. Most respondents identified Television (15%), followed by Friends, Relatives, and Social Media (13%), as the third-most important source of information (See Table 1).

COVID-19 RECOMMENDATIONS & TESTING
Ninety-three percent of respondents reported following pandemic recommendations and 7% reported they were not following recommendations. Only 2% of respondents had received a test for COVID19. Table 2 displays why respondents had not received a COVID-19 test. The largest percentage was among respondents who said they didn't need a test (84%), but the test being unavailable was the second largest percentage (12%). Respondents were able to identify multiple reasons.'(See Table 2, next page).''
ANXIETY & DEPRESSION
Respondents who felt anxiety or depression because of COVID-19 were asked if they were able to access emotional support or services. Eighty percent of respondents reported having access to emotional support or services and 20% reported not having access.'
ACCESS TO DIRECT CARE WORKERS & REGULAR HEALTH CARE
Respondents were asked if they used a Direct Care Worker (e.g., Home Health Aide, Personal Care Aide, or Unpaid Family Caregiver), if this care continued during the pandemic, and if respondents had been able to maintain a safe distance from their Direct Care Worker (e.g., six feet). Seventytwo percent of respondents received Direct Care Worker services and 76% of respondents continued to receive these services during the pandemic. But only 50% of respondents were able to maintain a safe distance from Direct Care Workers.
ACCESS TO REGULAR HEALTH CARE TREATMENT & PRESCRIPTIONS
Many persons with disabilities receive regular health care treatment such as physical therapy, dialysis, bloodwork, etc. Among respondents who needed regular health care, 56% reported access had been disrupted and 44% reported that access had not been compromised. Among respondents taking prescriptions, 98% reported that access had not been affected and 2% reported access had been disrupted. Thirty-eight percent of respondents reported experiencing new challenges to accessing health care.
DISCUSSION
One of the limits of using a convenience sample is that results cannot be generalized to a larger population, although they can be informative for planning purposes and, in particular, assessments of health care quality (Bethell, et al, 2004). Below, we discuss observations about the survey results in relation to the sample.
COVID-19 Information & Impact: Several important findings emerged from the information and impact survey questions. Relatives were an important COVID19 information source whether as the most important, second-most important or third-most important source, as well as Television and, to slightly lesser extent, the Internet. This suggests an important role for parents and families in communicating information about the pandemic and how public health and health care professionals need to be represented on television in order to provide credible information on how to respond to the pandemic.
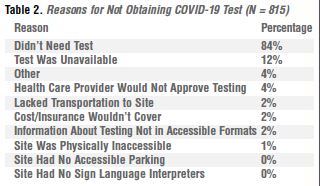
While several national polls report varying levels of endorsement for COVID-19 guidelines, this sample reported high levels of compliance with guidelines at 93%. This suggests that this sample is taking the risks of the coronavirus pandemic very seriously. Echoing national findings, only a small percentage (2%) of respondents had received a COVID-19 test. Of concern is that 12% of persons had not received a COVID-19 test because the test was unavailable and, to a lesser extent, that health care providers would not authorize the test (4%). These may become more acute issues (at least for this sample) as the impact of the pandemic continues over time. Similarly, although 66% of respondents were experiencing anxiety or depression as a result of the pandemic, 20% lacked access to emotional supports/services. Emotional issues could grow among other respondents over time as the pandemic continues and lack of services/supports may make these problems more acute.
Access to Regular Health Care & Services: A high proportion of the sample used Direct Care Worker services (72%). While a majority of respondents (76%) continued to receive these services during the pandemic, the loss of these services among 24% of the sample could contribute to major problems.'Moreover, the lack of safe distancing among 50% of respondents could increase infection rates. Clearly, safeguarding information is needed by a substantial proportion of the sample.
Of concern is that 56% of respondents experienced disruptions in their regular health care treatment services during the coronavirus pandemic. Ensuring needed health care for the respondents is an important but challenging problem. In contrast, 98% of respondents taking medications reported that they could access their prescriptions. Yet, for the 2% of the sample who had prescription medication access disrupted, this representants a potentially life-threatening situation. Moreover, 38% of the sample reported experiencing new challenges to obtaining health care treatment, health care access, and/or prescriptions. In many ways, the novel coronavirus pandemic is presenting unfamiliar and unanticipated challenges for persons with and without disabilities.'A key difference is that persons with disabilities already encounter documented disparities in accessing health care treatment and services (Krahn et al., 2015). A careful analysis of the open-ended responses describing the new barriers is underway.
Limitations: The findings in this report are subject to a number of limitations. The sample is atypical from population-based disability samples on a number of dimensions. The overall sample includes a higher than typical proportion of persons with intellectual disability, autism, epilepsy, or brain injury (as the underlying condition contributing to DCRD), is younger, predominately female, White, and Suburban (47%), and has some type of insurance. The survey data are also self-reported and may be subject to reporting or recall bias. The responses represent a snap shot between April 17, 2020, until May 1, 2020, and the coronavirus pandemic situation has changed since these responses were given. Lack of internet access may bias the sample and persons with multiple disabilities may not be accurately identified since we asked for a person's "main" disability. Finally, because of the use of a convenience sample, the results are not generalizable to the overall population of persons with intellectual disability, autism, epilepsy, or brain injury.
CONCLUSION
The results of this survey provide insights into a moment in time during the coronavirus pandemic.'The challenges revealed for this sample need to be examined with population-based research, and tracked over time. Moreover, the intricacies and changing dynamics of the pandemic establish a critical need for policy and programmatic responses to this extraordinary health and public health challenge.
Acknowledgements: Funding for this research was provided by the Bristol Myers Squibb Foundation. Contents are solely the responsibility of the authors and do not necessarily represent the official views of the Bristol Myers Squibb Foundation. (Published with Permission from the AAHD)
ABOUT THE AUTHORS:
Charles E. Drum, MPA, JD, PhD., is the founding Director of AAHD's National Center on Research, Knowledge Translation, and Dissemination.'Prior to joining AAHD, he had a 30-year career in academia and is a national and internally known expert in health and disability, specifically in health disparities, access to care, health promotion research, and knowledge translation. Anthony Oberg, MA, is a Project Associate and Accessibility Specialist with AAHD, where he coordinates a training project and ensures the accessibility of AAHD materials. Jacob Ditsch, OTD, is a Project Associate with AAHD, where he coordinates the Venous Thromboembolism project. Karl Cooper, JD is an attorney, disability advocate, and Director of Public Health Programs at AAHD. He specializes in training, technical assistance, and dissemination activities at AAHD and leads several disability and public health initiatives. Roberta Carlin, MS, MA, JD., has been Executive Director of AAHD since 2002. She has been involved in the disability and health field for over 30 years working in the areas of health promotion, disability research, women's health, community engagement and community inclusion, strategic information dissemination and knowledge translation, stakeholder engagement, and emergency preparedness.
References
Bethell, C., Fiorillo, J., Lansky, D., Hendryx, M., & Knickman, J. (2004). Online consumer surveys as a methodology for assessing the quality of the United States health care system. Journal of Medical Internet Research, 6(1), e2. doi.org/10.2196/jmir.6.1.e2 Krahn GL, Walker DK, Correa-De-Araujo R. (2015). Persons with disabilities as an unrecognized health disparity population. Am J Public Health. 2015 Apr;105 Suppl 2:S198-206. doi: 10.2105/AJPH.2014.302182. Epub 2015 Feb 17. White, GW. (2009). Nobody Left Behind: Disaster Preparedness and Public Health Response for People with Disabilities. In Drum, C.E., Krahn, G.L., & Bersani, Jr., H. (Eds.), Disability and Public Health. Washington, DC: American Public Health Association & American Association on Intellectual and Developmental Disabilities.