We, along with many other healthcare advocates and organizations, believe a nationwide systemic change is needed to ensure all health care professionals have mandatory training about people with IDD.
LET'S MAKE THE UNFAMILIAR FAMILIAR!
BY ELIZABETH PERKINS PHD RNLD FAAIDD FGSA AND SETH VANZANT MD, MPH

GETTING TO KNOW YOU: FCIC's approach has been to produce health advocacy resources that can empower the person with IDD, their families, and their health care provider to know more about each other, and bridge the communication and knowledge gaps that can exist on a 1:1 basis.
This article highlights a range of free health resources available from the Florida Center for Inclusive Communities (FCIC), a University Center for Excellence in Developmental Disabilities, at the University of South Florida. They were designed to improve health care encounters for people with intellectual/developmental disabilities, their family members, and their health care providers.
People with intellectual/developmental disabilities (IDD) are a unique population – they are more likely to have multiple health conditions, they are often disadvantaged in being able to access good quality care, and even more frustrating, is the fact that the vast majority of health care professionals receive very little training on how to best support and communicate with people with IDD. Inadequate training can amplify feelings of apprehension and awkwardness from health care professionals, through no fault of their own. Poorly prepared professionals can leave people with disabilities feeling dissatisfied with their health care encounters.
We, along with many other healthcare advocates and organizations, believe a nationwide systemic change is needed to ensure all health care professionals have mandatory training about people with IDD. Such initiatives are already underway, though they will take some time to implement, as skills and competencies need to be developed, agreed, and endorsed. Furthermore, implementation into already dense training curricula in medical, nursing, physical therapy, and other allied health professions, will ultimately mean that "something's gotta give" i.e. coverage of some other topic will need to be reduced or removed to make space. Buy-in from licensing and accreditation bodies will also need negotiating. It's certainly a long road ahead.
So what can we do in the meantime? How can we make the FCIC provides training to medical, nursing, and students in other allied health professions, and continuing education to those already in the field.
Beyond that, our approach has been to produce health advocacy resources that can empower the person with IDD, their families, and their health care provider to know more about each other, and bridge the communication and knowledge gaps that can exist on a 1:1 basis. Indeed, the introduction of these resources by a person and family member has resulted in not just one health care provider using them, but their subsequent adoption in numerous clinics, hospitals, even state-wide systems!
RESOURCES TO PROMOTE BETTER COMMUNICATION
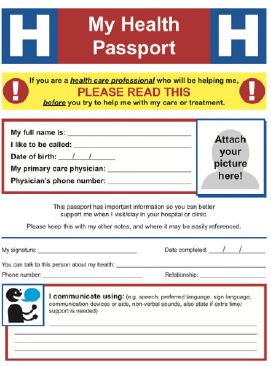
MY HEALTH PASSPORT
One of our most popular resources is My Health Passport ( flfcic.fmhi.usf.edu/docs/FCIC_Health_Passport_Form_Typeable_English.pdf) — a four-page document that was designed for when people with IDD are needing in-patient hospital care (e.g. for surgery, diagnostic screening etc.), and may need to spend a few days in hospital with staff who are very unfamiliar with them. It is designed to be shared with many types of healthcare providers, in clinic and hospital settings, especially for those who are not very familiar in providing care to individuals with IDD. It describes the unique supports and preferences of an individual. My Health Passport is completed by the patient/caregiver and then shared with their health provider.
My Health Passport has been endorsed by the American Academy of Developmental Medicine and Dentistry (AADMD), and the Developmental Disabilities Nurses Association (DDNA). "Successful patient care can often be hampered by having inadequate personal and health information between the individual with developmental disabilities, their family and caregivers, DSP's and other agency staff, and the healthcare provider. My Health Passport is a wonderful document that contains basic and essential health information as well as personal characterizations of the individual. I highly recommend it." Seth Keller, MD - former President of AADMD.
MY HEALTH REPORT
My Health Report ( flfcic.fmhi.usf.edu/docs/FCIC_My_Health_Report_Fillable.pdf) is two-page document to be used for primary care appointments with a person's family doctor. It was designed for adults with IDD, with feedback from family physicians to help individuals and family caregivers give relevant health information as efficiently as possible. It is designed to contain information to help to quickly establish the reason for the visit, prompt the patient/ family remember information about their symptoms, leaving more time to be available for discussion and treatment options. The form also reminds the physician to enquire about overall health status too.

Developing these types of resources is a careful balancing act between keeping it user-friendly to people with disabilities and their family caregivers, while at the same time providing pertinent information to the healthcare professional. As such, it is vital that resources are developed in conjunction with and feedback from people with IDD, family members of people with IDD, and medical professionals with high caseloads of people with IDD to ensure such utility. Overall, our health advocacy resources serve three different objectives - i) to improve communication and knowledge between specific patients with IDD and their healthcare professionals, ii) to empower individuals to learn more about health, and iii) to improve provider knowledge about disability.
We hope you use and share these resources with your healthcare providers, and health advocacy activities with others. Help us to make the unfamiliar familiar! •
Learn more at FCIC's Health Resources page: flfcic.fmhi.usf.edu/program- areas/health.html?tab=2
ABOUT THE AUTHORS:
Elizabeth Perkins PhD RNLD FAAIDD FGSA is the Associate Director and a Research Associate Professor at the Florida Center for Inclusive Communities UCEDD, at the University of South Florida. Originally from Great Britain, Dr. Perkins is also a Registered Nurse in Learning Disabilities (the equivalent of intellectual disabilities). She is the immediate Past President of the American Association on Intellectual and Developmental Disabilities. Dr. Perkins welcomes any comments, suggestions, and feedback about FCIC's health resources at eperkins@usf.edu Seth VanZant MD, MPH is a resident physician in the neurodevelopmental disabilities program at the UPMC Children's Hospital of Pittsburgh. His research interests include the provision of care and health advocacy for patients with intellectual and developmental disabilities. He is an active member of the American Academy of Pediatrics Section on Children with Disabilities and the American Public Health Association Disability Section. While pursuing his MD at the Morsani College of Medicine, at the University of South Florida, Dr. VanZant was mentored by Dr. Perkins in their FCIC UCEDD Trainee/Mentorship program.
RESOURCES TO EDUCATE PEOPLE ABOUT HEALTH
EDUCATION FOR LIFELONG HEALTH AND LIFELONG MENTAL HEALTH FACTSHEETS
These factsheets were designed as educational resources for people with mild intellectual disability. Usual treatments and prevention tips are also highlighted. Current topics available are:
Anxiety flfcic.fmhi.usf.edu/docs/ELMH_Anxiety.pdf
Cancer flfcic.fmhi.usf.edu/docs/FCIC_EFLH-4-Cancer%20Fact%20sheet.pdf
Cancer Treatment flfcic.fmhi.usf.edu/docs/FCIC_EFLH-5-Cancer%20Treatment%20Fact%20sheet.pdf
Depression flfcic.fmhi.usf.edu/docs/ELMH_Depression.pdf
Diabetes flfcic.fmhi.usf.edu/docs/FCIC_EFLH-2-Diabetes%20Fact%20sheet.pdf
Good Health and Hygiene flfcic.fmhi.usf.edu/docs/FCIC_EFLH-1-Hygiene%20Fact%20sheet.pdf
Osteoporosis flfcic.fmhi.usf.edu/docs/FCIC_EFLH-3-Osteoporosis%20Fact%20sheet.pdf
Seizures & Epilepsy flfcic.fmhi.usf.edu/docs/FCIC_EFLH_7_Epilepsy.pdf
How Do I Talk to My Doctor? flfcic.fmhi.usf.edu/docs/FCIC_EFLH-6-TalkingToMyDoctor_Fact%20sheet.pdf
RESOURCES TO IMPROVE PROVIDER KNOWLEDGE
We also believe in being proactive and helpful to healthcare providers and staff who will come into contact with people with IDD. Many may have received little-to-no actual training about disability in general, and especially concerning adults and older adults with IDD. The most fundamental aspect we emphasize is how communication can be improved, along with useful but brief guidance to facilitate better awareness. Our factsheet Improving Communication with Patients who have Intellectual and Developmental Disabilities ( flfcic.fmhi.usf.edu/docs/FCIC_PhysicianFactSheet_1_Improving_Communication.pdf) provides an overview of why healthcare providers need to pay much more attention to this population, ways to improve communication and build rapport, guidance on how to conduct appropriate physical examinations as well as referencing scholarly articles for those interested in further research into this topic.
Excelling in care for patients with DD through communication, environment, and logistics, i.e. XCEL ( xcel.flcic.org) is an entertaining 8-minute video resource that is designed for all types of health and support staff who may encounter people with DD in healthcare settings. There are handy hints on how to communicate appropriately, how to be mindful of how the environment can be modified to be more welcoming and inclusive of peo ple with disabilities, and how we can help make appointments more convenient for people with IDD. There is also an accompanying factsheet — to help reinforce and remind people of the major points highlighted in the video, as well as more in-depth resources for those seeking further information.