BY LAUREN AGORATUS, M.A.
Families are finding that even if they have private insurance coverage as their primary coverage, if they have Medicaid as secondary coverage, some providers are turning their children away. This is due to a misunderstanding on how Medicaid can be billed. If providers accept children with disabilities who have both private and public coverage, this is mutually beneficial.

BETTER ACCESS: Using Medicaid as secondary insurance could result in better health outcomes, benefitting both providers and families.
How Medicaid Helps Children with Special Needs
According to Medicaid.gov, 27 million children under age 18 are covered by Medicaid. Half of children with special health care needs are covered by Medicaid.1 Medicaid often offers more benefits than employer plans. This is due to the EPDST (Early and Periodic Screening, Diagnostic, and Treatment) provision. This means:
•"Early: Assessing and identifying problems early
• Periodic: Checking children's health at periodic, age-appropriate intervals
• Screening: Providing physical, mental, developmental, dental, hearing, vision, and other screening tests to detect potential problems
• Diagnostic: Performing diagnostic tests to follow up when a risk is identified, and • Treatment: Control, correct or reduce health problems found." 2
• Treatment: Control, correct or reduce health problems found." 2
Why Provider Offices May Turn Families Away
Providers may be concerned that if a child has Medicaid, they won't get the full payment. However, private insurers pay the same amount they would have paid whether or not the patient has Medicaid. There are options for providers to receive the remaining balance. Nonparticipating providers can, but don't have to, bill Medicaid as secondary out-of-network which lessens the burden on parents. Providers may opt instead to bill families.
What Can Families Do?
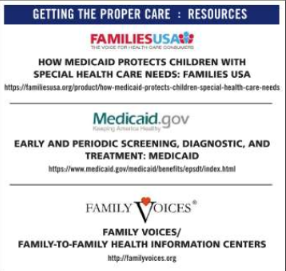
Parents can contact the billing department in the provider's office to discuss options. They can let them know that they can bill out-of-network as secondary coverage. Families can also sign a form indicating that they agree to be balance-billed for whatever isn't covered. That way everyone is on the same page: the family isn't unnecessarily turned away due to billing issues and the provider knows they'll get full payment. Some families may opt not to show their Medicaid card, in which case they can be held responsible for the remaining balance. If parents are having problems accessing care, they may wish to contact Family Voices/Family-to-Family Health Information Centers in their state (see Resources).
COMMENTS FROM PROVIDERS:
"For children with medical complexity there's a reasonable likelihood that there is access to social work or a care coordinator who can help identify additional resources or 'go to bat' that will help gain access to providers."
"The ability to advocate will be essential, if not to solve the problem, but to raise awareness. Also consider reaching out to family-based organizations that advocate at the statewide or national level regarding access to care and recognize your voice may be needed to promote change. If you are unable to access a necessary service due to a lack of providers accepting Medicaid, state and federal lawmakers and regulators need to hear from you."
Exception
If an individual has both Medicare and Medicaid, this does not apply. These individuals are known as "dual eligible". In this case, providers may not balance-bill Medicaid for what Medicare doesn't cover. Balance-billing is prohibited by Federal Law Section 1902(n) (3) (B) of the Social Security Act. It states "(n) (3) In the case in which a State's payment for Medicare cost-sharing for a qualified Medicare beneficiary… (B) the beneficiary shall not have any legal liabil Medicaid, this does not apply. These individuals are known as "dual eligible". In this case, providers may not balance-bill Medicaid for what Medicare doesn't cover. Balance-billing is prohibited by Federal Law Section 1902(n) (3) (B) of the Social Security Act. It states "(n) (3) In the case in which a State's payment for Medicare cost-sharing for a qualified Medicare beneficiary… (B) the beneficiary shall not have any legal liability to make payment to a prov ider…"3 There are also state protections but some this in states only applies if the provider participates in Medicaid.4 In a d d i t i o n , providers may bill State Medicaid agencies for Medicare cost-sharing amounts.5 However, Medicare benefits are usually generous, and if the provider accepts Medicare they usually won't turn a family away.
Many children with disabilities have Medicaid as their secondary insurance and this approach can help remove obstacles to getting care. Also, a child with special needs may get more comprehensive care utilizing Medicaid due to the EPSDT provision. Using Medicaid as secondary insurance could result in better health outcomes, benefitting both providers and families.•
ABOUT THE AUTHOR: early and Periodic screening, diagnostic, and treatMent: Medicaid medicaid.gov/medicaid/benefits/epsdt/index.html Lauren Agoratus, M.A. is the parent of a child with multiple disabilities who serves as the Coordinator for Family Voices-NJ and as the central/southern coordinator in her state's Family-to-Family Health Information Center, both housed at SPAN, found at spanadvocacy.org
References FaMily Voices/ FaMily-to-FaMily HealtH inForMation centers familyvoices.org 1. familiesusa.org/product/how-medicaid-protects-children-special-health-care-needs 2. medicaid.gov/medicaid/benefits/epsdt/index.html 3. ssa.gov/OP_Home/ssact/title19/1902.htm 4. justiceinaging.org/wp-content/uploads/2017/02/Fighting-Improper-Billing-of-Dual- Eligibles-New-Strategies.pdf 5. cms.gov/Outreach-and-Education/Medicare-Learning-Network- MLN/MLNMattersArticles/downloads/SE1128.pdf